Lee, B.C., Moody, J.B., Poitrasson-Rivière, A. et al. Blood pool and tissue phase patient motion effects on 82rubidium PET myocardial blood flow quantification. J. Nucl. Cardiol. 26, 1918–1929 (2019).
Description:
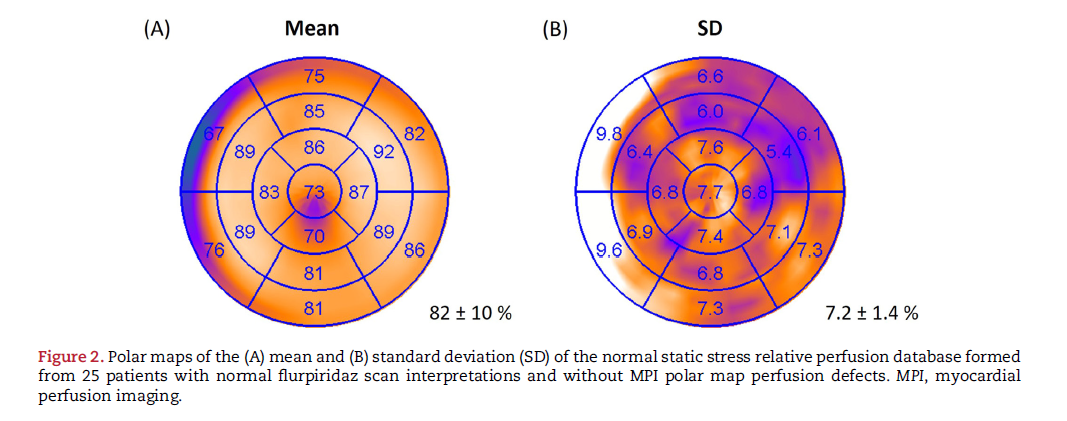
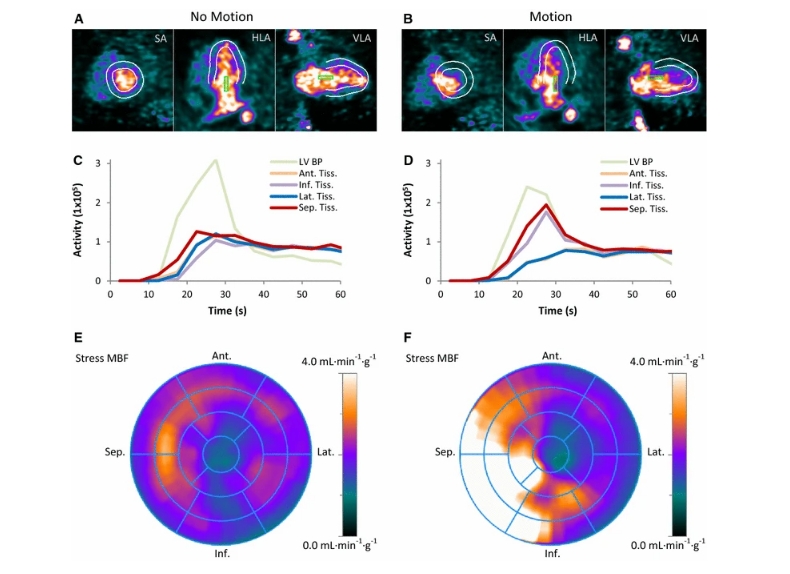
This study investigated the prevalence and impact of patient motion on myocardial blood flow (MBF) and myocardial flow reserve (MFR) quantifications in dynamic PET myocardial perfusion imaging using rubidium-82 chloride (82Rb). Analysis of 225 consecutive patients revealed that mild to moderate motion (5-15 mm) occurred frequently during the blood phase, particularly in the septal and inferior directions. The study showed that motion during this phase led to significant errors in MBF and MFR estimates, notably in the RCA territory when motion was in the inferior direction.
Clinical Relevance:
Accurate quantification of MBF and MFR is crucial for the diagnosis and management of coronary artery disease.
This study highlights the significant impact of patient motion, especially during the blood phase, on these measurements. Recognizing the prevalent nature of this motion and its directional impact assists in understanding measurement inaccuracies and underscores the necessity for targeted motion correction strategies. Implementing such corrections will likely improve the reliability and diagnostic accuracy of PET myocardial perfusion imaging, ultimately enhancing patient management and treatment outcomes.
Partners in Research:
INVIA Medical Imaging Solutions and the University of Michigan collaborated on this research.